RETINA
DRY EYE
OCULAR HEALTH
ACUTE CARE

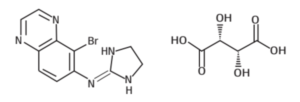
MOXNEALTM
Moxifloxacin Eye Drops I.P.
0.5% w/v
0.5% w/v

MOXNEAL-LTM
Moxifloxacin and Loteprednol Etabonate Ophthalmic Suspension
0.5% w/v + 0.5% w/v
0.5% w/v + 0.5% w/v

NEPANEALTM
Nepafenac Ophthalmic Suspension
0.1% w/v
0.1% w/v

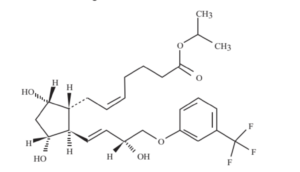
LOTENEALTM
Loteprednol Etabonate Ophthalmic Suspension
0.5% w/v
0.5% w/v

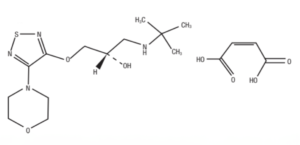
OLONEALTM
Olopatadine Ophthalmic Solution I.P.
0.2% w/v
0.2% w/v